Breastfeeding is a wonderful gift to be able to share with your baby, but it is a learned skill (for both mother and baby) that does have its challenges. Mastitis is a really common issue for breastfeeding mothers, with around 17% experiencing mastitis in the first 6 months after birth. Unfortunately, it is also a common cause of women ending the breastfeeding relationship earlier than they would like to. This blog is designed to give you the tools and information you need to address mastitis from a naturopathic approach so you can get back to pain-free feeding.
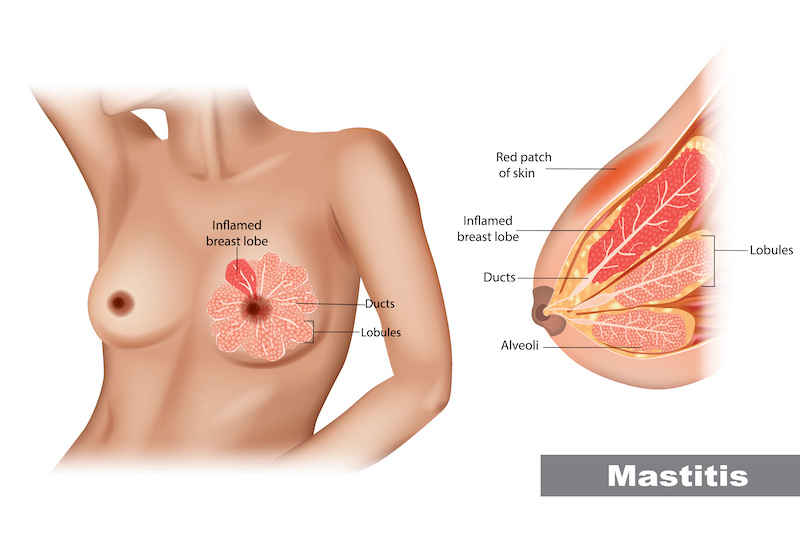
So, what is mastitis? Mastitis is an inflammation and/or infection of the breast tissue. It is often due to an underlying blocked duct, and there may or may not be an infection involved. 75-95% of mastitis cases happen during the first 12 weeks of breastfeeding. This is the time during which your body is still regulating supply, which can mean fluctuating milk production levels throughout the day or week.
Symptoms of mastitis include:
- Pain
- Swelling
- Redness of the breast
- Reduced milk production
- A general feeling of being unwell
- Fever
Mastitis can develop and progress very quickly. Without adequate treatment, it may also progress to abscess formation. It’s important to begin treatment for mastitis as soon as symptoms appear to avoid progressing to severe symptoms like a high fever or abscess, which would require urgent medical care.
Causes and Risk Factors
There are a number of underlying causes and risk factors that can contribute to mastitis developing, including:
- Blocked or clogged ducts
- Cracked nipples
- Antibiotic use during pregnancy or breastfeeding
- Attachment and feeding issues, including poor latch or positioning of baby during feeds
- Delayed feeding
- Incomplete emptying of breasts during feeds
- Infrequent nursing, or reduced frequency of feeds
- Oversupply (can be simply due to your body’s overproduction of milk, or can be due to pumping in between feeds)
- First pregnancy
- Age (either under 21 or over 35)
- Poor gut health and dysbiosis
- Compromised immune health
- Wearing tight-fitting bras
When looking to prevent future recurrence, it’s important to address any of the above factors which may have contributed to mastitis developing.
Naturopathic Understanding of Mastitis
Human breast milk naturally contains its own microbiome, in the much the same way as the gut and skin. The good bacteria in breast milk help to maintain the health of the ducts by preventing other bacteria to grow – such as the Staphylococcus bacteria which are associated with mastitis. Naturopathically, we understand that mastitis can be a presentation of dysbiosis (imbalance of the body’s bacterial populations) – the good bacteria naturally found in breastmilk have become outnumbered by the harmful bacteria, resulting in infection, and leading to inflammation and illness. Immune system suppression also frequently plays a role – new mothers’ bodies are under significant stress, with postpartum healing, balancing the mental and emotional stressors of motherhood, and sleep deprivation, too. All of this can cause the body’s defences to become depleted and less able to protect against infection and inflammation.
Naturopathic Treatment Strategies for Mastitis
Dietary Strategies
Avoid Foods that Suppress Immune Function
Healing mastitis requires a robust response from the immune system. Certain foods can supress immune function and so are best avoided during this time. Foods that suppress immune system function include:
- Caffeine – particularly as found in coffee and energy drinks. The caffeine in tea is largely counteracted by the beneficial effects of L-theanine, an anti-inflammatory and immune-boosting amino acid that naturally occurs in tea
- Alcohol
- Deep fried foods and foods high in saturated fats, including chips and many packaged snack foods
- Foods high in trans fats, including cakes, muffins, frozen ready-foods (such as chips and pizza)
- Foods high in sugar, such as chocolate, lollies, baked sweet foods, and soft drinks
Keep hydrated
Adequate hydration is vital for a healthy immune system and for milk production. We need plenty of water to keep our lymphatic fluid moving properly through the body – this is how our immune cells travel around the body. Keeping hydrated is doubly important during mastitis, as we need both milk production and lymphatic flow to help clear any duct blockages that are present. Aim for 2.5-3L of water per day, plus extra when exercising or sweating. In cold weather, or when you’re feeling unwell, it can be difficult to drink this much water cold. Hot tea (including herbal tea) can be a great alternative to keep up your fluid intake – check the “herbal medicines” section of this handout for herbal tea options suited for mastitis.
Eat Well-Cooked, East to Digest Foods
Well-cooked and easy-to-digest foods are ideal, as these foods are easier for your body to break down and absorb vital nutrients. Soups, stews, and slow-cooked curries are all great options, which you can load up with immune-boosting vegetables, herbs and spices, and good quality protein sources. These types of meals are also great options for batch cooking – you can cook large portions and freeze leftovers for later meals.
Eat Protein with Every Meal
Protein forms the building blocks for cells, including immune cells. It is a vital part of a healthy immune system, and we have higher protein requirements during illness. Some good sources of protein include:
- Red meat, like beef, lamb, and kangaroo. Try cooking in a slow cooker until tender, as it will be easier to digest.
- Poultry, including chicken and turkey. Try roasted or baked, and add to soups
- Legumes – lentils, kidney beans, black beans, chickpeas, and more. Be sure to thoroughly soak and wash before cooking, and always cook them until soft – this will ensure they are much easier to digest. Legumes are a great protein option to use in curries and stews.
- Tofu and tempeh – both of these are highly versatile and can be used in curries, soups, stews, and even broths – a low-sodium miso soup with tofu or tempeh and some dried kelp or wakame (seaweed) can be a good, warming option when you have a low appetite. Miso paste is readily available at health food stores and provides a good dose of probiotics to your diet.
- Eggs – free range eggs can be boiled, scrambled, or poached
- Fish – baked, grilled, or even added to curries, fish and other seafoods can be a great addition.
Include Antimicrobial Foods
Loading up on antimicrobial foods can give your immune system a helping hand when it comes to fighting off bacterial infections such as mastitis. Some easy options to add include:
- Garlic, onions, and shallots – can be added to virtually any savoury dish!
- Mushrooms – shiitake and oyster mushroom varieties are frequently available in supermarkets and have great immune-boosting and antimicrobial properties
Supplements and Herbal Medicines
Every mum is different, and a tailored treatment plan will ensure a strategic prescription however some of the more common recommendations include:
Vitamin C
Specific Probiotic strains & prebiotic fibres
Herbal medicines can be a really useful tool with mastitis, helping to support the immune system, promote lymphatic circulation to improve breast duct clearance, as well as providing symptomatic relief. Below are some examples of herbs that may be used in your treatment plan. If a herbal tincture is provided for oral use, instructions will be provided and may include Echinacea, Poke Root, Oats Green and Comfrey and Parsley Leaf for use as a compress.
Lifestyle Strategies
- Apply warm compresses to the affected area and take warm showers
- Hand express or pump before or after feeding to relieve pain, if needed, or if baby won’t feed on that side
- Use an ice pack after feeding to reduce swelling.
Prioritise Rest
It’s important to rest as much as possible, to give your body the time it needs to heal. This is especially important if you are still breastfeeding frequently at night and have broken sleep. Both sleep and rest are crucial for healing! Delegate tasks wherever possible, batch cook meals to reduce time spent preparing food, and take the opportunity to nap or rest whenever you can. You can also help to get more restorative sleep at night by turning off overhead lights (use low-light lamps instead) and switch off screens at least an hour before bed each night.
Continue to Feed Baby Often
Continue to feed baby as normal, focusing on draining the breast. It is fine to continue to feed on the mastitis-affected breast, so long as it is not too painful to do so!

Self-Massage
Gently massage the area with oil in between feeds, making sure to wipe off excess oil before you next feed baby. Massage in a circular motion working towards the nipple. This will help to improve circulation and encourage clearance of any blocked ducts. You may also wish to do this while in the shower, as the warm water will further boost circulation and clearance. You can use a pokeroot salve, calendula oil, comfrey oil, or even plain coconut oil to massage.
Use Warmth to Relieve Pain
Warm showers and warm compresses can help to relieve pain and reduce inflammation. A cloth soaked in warm water will do, or a herbal compress like those detailed in the “herbal medicines” section above.
Relieve Pain from Fullness
Hand-express or pump as needed to relieve pain, especially if baby won’t feed from that side. Be sure not to overdo it, though – you don’t want to stimulate more milk production.
Ice Pack for Swelling
If you are experiencing swelling, an ice pack wrapped in cloth applied to the breast will help.
To Reduce Oversupply
If oversupply is an underlying cause of your mastitis, the following tips might help:
- Apply frozen cabbage leaves to your breasts in between feeds – this is also very soothing!
- Drink 3 cups of sage tea per day – discontinue once your supply has balanced out
- Avoid pumping in between feeds – feed baby as needed and always aim to fully drain the breast before moving baby to the next breast. If you are prone to oversupply issues, avoid using a Haka or pump on the other side to catch the “overflow”, as this can signal to the brain to increase supply.
Book in to see me (Tanya Edwards) for Naturopathic support
If you’re struggling with mastitis and breastfeeding your baby, getting some professional guidance can be helpful. A naturopathic consultation is a good start to help find the best treatment for you. To find out more, contact Performance in Health today.
References
Amir, L. H., Forster, D. A., Lumley, J., & McLachlan, H. (2007). A descriptive stud of mastitis in Australian breastfeeding women: Incidence and determinants. BMC Public Health, 7(62).
Angelopoulou, A., Field, D., Ryan, C. A., Stanton, C., Colin, H., & Ross, R. P. (2018). The microbiology and treatment of human mastitis. Medical Microbiology and Immunology, 207, 83–94.
Barker, M., Adelson, P., Peters, M. D. J., & Steen, M. (2020). Probiotics and human lactational mastitis: A scoping review. Women and Birth, 33(6), 483–491.
Beim, M. (2022). Mastitis. https://mimbeim.com/mastitis/
Hurtado, J. A., Maldonado-Lobon, J. A., Diaz-Ropero, M. P., Flores-Rojas, K., Uberos, J., Leante, J. L., Affumicato, L., Couce, M. L., Garrido, J. M., Olivares, M., & Fonolla, J. (2017). Oral administration to nursing women of Lactobacillus fermentum CECT5716 prevents lactational mastitis development: A randomized controlled trial. Breastfeeding Medicine, 12(4), 202–209.
Jimenez, E., Fernandez, L., Maldonado, A., Martin, R., Olivares, M., Xaus, J., & Rodriguez, J. M. (2008). Oral administration of Lactobacillus strains isolated from breast milk as an alternative for the treatment of infectious mastitis during lactation. Applied and Environmental Microbiology, 74(15), 4650–4655.
Ojo-Okunola, A., Nicol, M., & du Toit, E. (2018). Human breast milk bacteriome in health and disease. Nutrients, 10(11).
Red Moon Herbs. (2019). Clogged milk ducts and mastitis: Poke root to the rescue. https://redmoonherbs.com/blogs/womens-health-and-herbal-medicine/clogged-milk-ducts-and-mastitis-poke-root-to-the-rescue
Soto, A., Martin, V., Jiminez, E., Mader, I., Rodriguez, J. M., & Fernandez, L. (2014). Lactobacilli and bifidobacteria in human breast milk: Influence of antibiotherapy and other host and clinical factors. Journal of Pediatric Gastroenterology and Nutrition, 59(1), 78–88.
Valls-Belles, V., Abad, C., Hernandez-Aguilar, M. T., Nacher, A., Guerrero, C., Balino, P., Romero, F. J., & Muriach, M. (2022). Human milk antioxidative modifications in mastitis: Furhter beneficial effects of cranberry supplementation. Antioxidants, 11(1).
WIllson, K. (2022). Mastitis prevention and treatment. https://www.pbcexpo.com.au/blog/mastitis-prevention-treatment










