Anxiety is an incredibly common condition in this busy world in which we live. Both myself as a naturopath in Sydney and the mental health practitioners that practice from Performance in Health Wellbeing Clinic, support a range of individuals in Anxiety Management.
I also focus on digestive issues and IBS as a naturopath, and it is certainly an area of health that I am passionate about. I find that irritable bowel syndrome (IBS) is a diagnosis often via exclusion and once other health conditions have been excluded, IBS is the diagnosis given. This basically means that the actual cause of your gut distress is not known. It is important to exclude other causes which is always part of my treatment plan when working with gut related issues.
When I am supporting someone with an IBS diagnosis, I always consider anxiety as a cause. In saying this, I always assess for chronic constipation as the cause, slow gut motility, Post Infectious IBS, endometriosis on the colon, bacterial overgrowth in the small and/or large intestine, bacterial dysbiosis, food intolerances & malabsorption conditions and thyroid disease. I often recommend functional testing to delve more deeply into what is happening for my clients. Often Inflammatory Bowel Disease, GERD, H Pylori or more may have been excluded by a gastroenterologist.
I also find that it may be several health-related issues that may create the “perfect storm” of Chronic IBS.
What I do know without a shadow of a doubt is that in approximately 70% of case gut issues drive anxiety and in approximately 30% of cases anxiety drives gut issues however no matter where it starts, one drives the other so you end up in a gut – anxiety – gut- anxiety circuit and treatment must also focus on both for successful outcomes.
Let’s talk statistics about Anxiety Driven IBS.
Both IBS and anxiety are common health issues for adults in Australia. IBS affects around 1 in 5 of us, whilst 1 in 6 will experience an anxiety disorder in their lifetimes. It’s becoming increasingly well established that our mood and our gut health are intrinsically linked and, anecdotally, many of us are all-too-familiar with the gut-churning effect anxiety and stress can have on our bodies. We’ve previously discussed on the blog about the link between gut health and low mood issues such as depression. But what about other mental health conditions? Do these also affect our gut health? Today we look at anxiety and how it can drive IBS – the mechanisms behind this, as well as some simple strategies to help you manage your anxiety symptoms to improve your gut health.
IBS
Irritable bowel syndrome, also known as IBS, is a really common gastrointestinal condition, affecting around 15% of the general population. IBS is a chronic functional disorder, characterized by recurrent symptoms of abdominal pain and bloating, as well as constipation, diarrhea, or both. Despite being common, it’s a complex condition that involves a complicated interplay between gut microbiota, diet, pain receptor dysregulation, and mental health. It’s very common for people with IBS to have concurrent mental health conditions, such as anxiety and depression – up to 90% of people with IBS also have one or more mental health conditions. What’s more, IBS symptoms often worsen during periods of acute stress or exacerbations of existing mental health conditions, and treatment for mental health can lead to reduced IBS symptoms. Recent studies suggest that IBS is actually a disorder of a breakdown in gut-brain communication, rather than being a strictly gastrointestinal health condition.
Anxiety and the Gut
Have you ever been anxious about an event and found you suddenly had to go to the bathroom? Or, if you experience an anxiety disorder, do you find that gastrointestinal symptoms are an issue for you? You’re not alone. Anxiety is one of the most common mental health conditions in Australia; many of us have experienced an anxiety disorder ourselves or have seen a loved one go through it. Anxiety causes both psychological and physical symptoms, with gastrointestinal symptoms being some of the most common issues for those with anxiety. Whilst typical symptoms might include shortness of breath, sweaty palms, and palpitations, acute anxiety can also look like:
- Diarrhoea, constipation, or both
- Abdominal cramping or pain
- Nausea, indigestion, or heartburn
- Loss of appetite, or increased appetite
So, what is going on here? There are a few reasons why these symptoms occur.
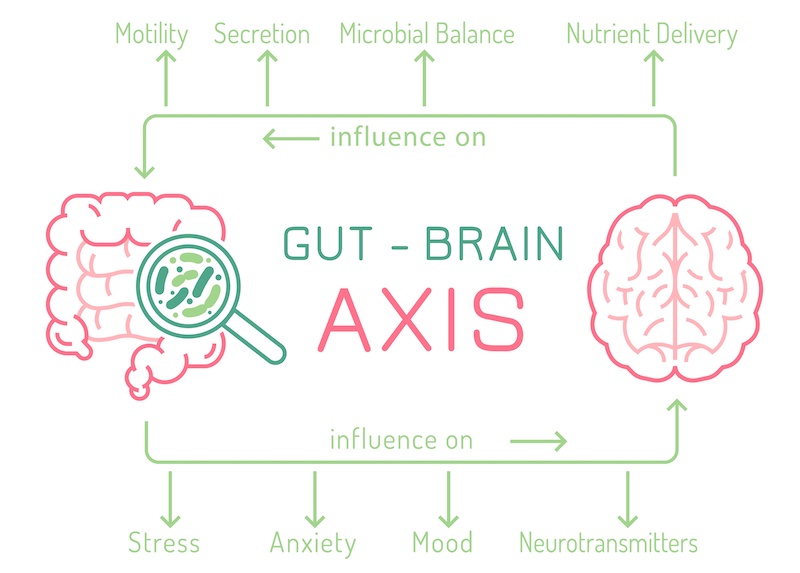
1. The Enteric Nervous System and The Gut-Brain Axis
The first reason for this link between anxiety and the gut is because both the gut and brain are connected via a system of nerves called the enteric nervous system (ENS), which is also known as the “second brain”, or the “gut-brain axis”. The enteric nervous system controls aspects of communication between the gut and the brain regarding functions such as digestion and gut motility. In fact, the vital functions of the gastrointestinal tract are almost entirely dependent on the enteric nervous system and things quickly fall apart if it is not working properly. Researchers have also found that the ENS may be responsible for some of the mood changes associated with gastrointestinal conditions like IBS. The ENS and gut-brain axis connects the emotional and cognitive centers of the brain with the gut. It is through this link that our thoughts and feelings affect our digestion and vice-versa.
2. The Physiology of Anxiety and Neurotransmitters
The second reason why anxiety and IBS are linked has to do with the chemical changes that occur in the body in anxiety. Physiologically, anxiety is essentially an overactivation of the fight or flight response, also known as the HPA axis or sympathetic nervous system. This means anxiety, like stress, puts our body into fight or flight mode. When the body is in fight or flight mode, “non-essential” functions such as digestion and immune function are suppressed. People with anxiety often aren’t digesting and absorbing their food adequately, particularly when symptoms are bad. What’s more, anxiety leads to altered levels of many important neurotransmitters, which are the chemicals the nervous system uses to send messages throughout the body. When neurotransmitter levels become altered, communication within the nervous system is compromised, as is communication between the brain and the gut via the ENS. Some of the neurotransmitters that are affected include noradrenaline, GABA, and acetylcholine, among others.
Noradrenaline
Noradrenaline, also known as norepinephrine, is a key neurotransmitter in the sympathetic nervous system (the fight or flight mode). It helps us to feel awake and alert and plays important roles in regulating our behaviour, memory, and learning. Anxiety typically causes noradrenaline levels to be higher than normal, which causes a fast heart right, high blood pressure, suppressed digestion, and slow bowels (meaning constipation). However, in periods of acute stress or anxiety, high noradrenaline can actually stimulate the bowels and trigger diarrhoea. In addition, noradrenaline can also cause alterations to the gut microbiota, leading to dysbiosis, which can make IBS symptoms even worse.
GABA
Gamma-aminobutyric acid (GABA) is our main calming neurotransmitter. Not only does it help us to feel calm, it is also important for helping with physical movement and cognitive function. Low GABA levels are typical in anxiety. Unfortunately, low GABA levels causes an increased sensitivity to pain in the gut, one of the most common symptoms in IBS. Low GABA levels can also negatively affect gut motility and the gut’s immune function, too.
Acetylcholine
Acetylcholine is another important neurotransmitter that is altered in both anxiety and IBS. Acute stress and anxiety cause low levels of acetylcholine in the gut and the brain, which leads to inflammation and increased gut motility, causing diarrhoea.
The Role of Gut Bacteria
Of course, we can’t discuss the gut without also discussing the gut microbiota. The gut microbiota is essential for the health of both the central nervous system (brain) and the ENS, because of the important neurotransmitters these bacteria produce, which are utilized by our nervous system. Bacteria in the gut produce not only serotonin, but also GABA, acetylcholine, and even melatonin. Animal studies show that changing the gut microbiota can trigger anxiety disorders and other mental health conditions, further highlighting how important our microbiota balance is. Gut bacteria directly affect the gut-brain axis, too. Bacteria communicate with nerve cells in the gastrointestinal tract, as well as communicating with the brain via the neurotransmitters they produce.
A Self-Perpetuating Cycle
It’s easy to see how the link between gut health and anxiety can lead to a self-perpetuating cycle for those with anxiety disorders and conditions like IBS. Once you are caught in this cycle, it will continue until both the anxiety and the gut aspects of your health are addressed. This is where as a naturopath I often make a significant difference in Anxiety Driven IBS through guiding you towards treatments that will help to address both the anxiety and the gut, to help make sure you are healing both parts of the issue.
Calming Your Anxiety for Better Gut Health
The good news is there are many ways you can start to gain control of your gut health by addressing your anxiety, and vice versa. Below are some great tips for helping to regain your health.
Herbal Medicines for Anxiety
Each person is unique and for this reason there are many herbs that I use for my KPI of Calm energy. This may also include herbs for more restorative sleep as sleep is critical for reducing next day anxiety. Some of my favourite herbs include kava, withania, rhodiola, passionflower, lavender and more.
Gut calming herbs
Again, this is dependent on medications and what is unique to each client however some of the herbs I may prescribe include chamomile, lemon balm, peppermint.
Use a Quality Probiotic when indicated
Prescribing a probiotic when someone actually has a bacterial overgrowth can worsen their symptoms when working with IBS. Once an overgrowth has been excluded and reasons for a lack of healthy gut bacteria has been identified then specific probiotics may be prescribed.
A good quality probiotic can be incredibly valuable in re-establishing a healthy gut microbiota for certain people. Certain specific microbial strains, such as Lactobacillius reuteri, have been found to improve gut motility and reduce pain perception in the gut, demonstrating good potential for use in IBS. However, remember that probiotic supplementation does need to be paired with prebiotics and a healthy, plant food-rich diet to ensure sufficient substrate available for bacterial populations to thrive. Unfortunately, many probiotics available on the market are of inferior quality or don’t contain therapeutic doses of specific bacterial strains that are beneficial for conditions like IBS. If you are interested in taking a probiotic, speak with your naturopath to find the right probiotic supplement for you.
Specific prebiotics
Many prebiotics can produce excess gas that worsen symptoms such as bloating and pain however proper prebiotic prescriptions made in line with symptoms can make a huge difference for symptoms and support good bacterial populations to grow.
Vitamin deficiencies and additional needs
Again, each person has different nutrient requirements depending on levels of stress in their lives including career, family, past history and more (which uses up nutrients), diet, lifestyle, and medications. Important nutrients for anxiety include magnesium, Zinc, Vitamin B, Vitamin C and more. The wrong magnesium at the wrong dose can worsen looser stools so be careful.
Blood sugar balancing
When supporting my clients with anxiety, a focus is always made around balancing blood sugar levels throughout the day and night as fluctuations can trigger and worsen anxiety. Having good energy levels throughout the day is also important as fatigue is a trigger for anxiety in many people.
Manage Your Stress
Finding ways to reduce your stress and improve your stress-coping skills can really help with anxiety. Stress management can be as simple as a daily 30-minute walk or starting a mindfulness practice.
Talk it Out
If you experience anxiety, having a professional you can talk to makes a big difference. If you don’t already, consider booking yourself in to see a psychologist, counsellor, or therapist, who can listen to your experiences and help direct you towards helpful strategies to manage your anxiety. Performance in Health Wellbeing clinic in Sydney’s Inner West have a team of well qualified professionals to help you.
Book in to see me (Tanya Edwards) for Naturopathic support
If you’re struggling to understand where to start, getting some professional guidance is key. A naturopathic consultation is an extremely thorough investigation which can help you to better understand your symptom picture and overall health as we work together to develop a holistic strategy to help you regain your health.
Treatment will look at what needs to be excluded. I may recommend a low FODMAP as a temporary measure to reduce gut symptoms as we figure out what is happening for you and herbs to reduce anxiety and gut issues at the same time. To find out more, contact Performance in Health today.
References
Annahazi, A., & Schemann, M. (2020). The enteric nervous system: “A little brain in the gut.” Neuroforum, 26(1).
Bercik, P. (2020). The brain-gut-microbiome axis and irritable bowel syndrome. Gastroenterology & Hepatology, 16(6), 322–324.
Carabotti, M., Scirocco, A., Maselli, M. A., & Severi, C. (2015). The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems. Annals of Gastroenterology, 28(2).
Cherpak, C. E. (2019). Mindful eating: A review of how the stress-digestion-mindfulness triad may modulate and improve gastrointestinal and digestive function. Integrative Medicine: A Clinician’s Journal, 18(4), 48–53.
Gros, M., Gros, B., Mesonero, J. E., & Latorre, E. (2021). Neurotransmitter dysfunction in irritable bowel syndrome: Emerging approaches for management. Journal of Clinical Medicine, 10(15).
Hadjivasilis, A., Tsioutis, C., MIchalinos, A., Ntourakis, D., Christodoulou, D. K., & Agouridis, A. P. (2019). New insights into irritable bowel syndrome: From pathophysiology to treatment. Annals of Gastroenterology, 32(6), 554–564.
Jerndal, P., Ringstrom, G., Agerforz, P., Karpefors, M., Akkermans, L. M., Bayati, A., & Simren, M. (2010). Gastrointestinal-specific anxiety: An important factor for severity of GI symptoms and quality of life in IBS. Neurogastroenterology & Motility, 22(6).
Lee, S., Wu, J., Ma, Y. L., Tsang, A., Guo, W.-J., & Sung, J. (2009). Irritable bowel syndrome is strongly associated with generalized anxiety disorder: A community study. Alimentary Pharmacology and Therapeutics, 30(6), 643–651.
Niesler, B., Kuerten, S., Demir, I. E., & Schafer, K.-H. (2021). Disorders of the enteric nervous system—A holistic view. Nature Reviews Gastroenterology & Hepatology, 18, 393–410.
Popa, S.-L., & Dumitrascu, D. L. (2015). Anxiety and IBS revisited: Ten years later. Clujul Medical, 88(3).
Shrestha, B., Patel, D., Shah, H., Hanna, K. S., Kaur, H., Alazzeh, M. S., Thandavaram, A., Channar, A., Purohit, A., & Venugopal, S. (2022). The role of gut-microbiota in the pathophysiology and therapy of irritable bowel syndrome: A systematic review. Cureus, 14(8).
Windgassen, S., Moss-Morris, R., Goldsmith, K., & Chalder, T. (2019). Key mechanisms of cognitive behavioural therapy in irritable bowel syndrome: The importance of gastrointestinal related cognitions, behaviours and general anxiety. Journal of Psychosomatic Research, 118, 73–82.










